Esophageal Manometry
Esophageal manometry is a test that shows whether your esophagus is working properly. The esophagus is a long, muscular tube that connects your throat to your stomach.
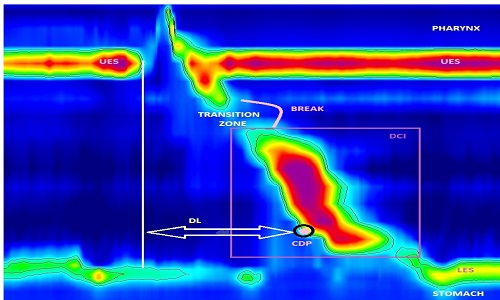
Esophageal manometry measures the rhythmic muscle contractions that occur in your esophagus when you swallow. The test also measures the force and coordination of esophageal muscles as they move food to your stomach.
During esophageal manometry, a thin, flexible tube that contains pressure sensors is passed through your nose, down your esophagus and into your stomach. Esophageal manometry can be helpful in diagnosing certain disorders that may affect your esophagus. Why it is done?
Your doctor may recommend esophageal manometry if you’re experiencing symptoms that could be related to an esophageal disorder.
Esophageal manometry provides information about the movement (motility) of food through the esophagus and into the stomach. The test measures how well the circular bands of muscle (sphincters) at the top and bottom of your esophagus open and close, as well as the pressure, strength and pattern of the wave of esophageal muscle contractions that moves food along.
If your main symptom is difficulty swallowing (dysphagia) or pain when swallowing (odynophagia), your doctor is likely to order other tests, such as X-rays, before or instead of esophageal manometry. These tests identify or rule out an obstruction in the esophagus — a narrowing, a complete blockage or an area of inflammation. Swallowing problems generally point more strongly to an obstruction than to a motility disorder.
Esophageal manometry may be used to help diagnose:
- Diffuse esophageal spasm. This rare swallowing problem is characterized by multiple, forceful, poorly coordinated muscle contractions of your esophagus.
- Achalasia. This uncommon condition occurs when your lower esophageal muscle (sphincter) doesn’t relax properly to let food enter your stomach. This can cause difficulty swallowing and regurgitation of food back up into your throat.
- Scleroderma. In many people with this rare progressive disease, the muscles in the lower esophagus stop moving, leading to severe gastroesophageal reflux.
If your doctor has recommended anti-reflux surgery to treat gastroesophageal reflux disease (GERD), you may need esophageal manometry to make sure you don’t have achalasia, which GERD surgery can’t help.
If you have chest pain not related to your heart, esophageal manometry may be recommended after an endoscopy to rule out GERD.


